What is diabetic retinopathy?
Diabetic retinopathy is a condition in the eye that occurs after many years of high blood sugar (diabetes mellitus). It consists of damage to tiny blood vessels within the retina resulting in abnormal leakage of fluid and blood inside the eye. If not detected or treated, diabetic retinopathy may cause macular edema (swelling), bleeding, scar tissue formation, retinal detachment, and blindness. Rarely, visual hallucinations may occur.
What is the retina?
The retina is a thin layer of delicate nerve tissue, which lines the inside wall of the eye like the film in a camera. In the eye, light is focused onto the retina, which “takes the picture” and sends the image to the brain. The retina has two main areas. The macula is the central area that gives you sharp, central vision and color vision. The peripheral retina is the part of the retina that gives you side vision and night vision.
What is diabetes mellitus?
Diabetes mellitus is a group of conditions characterized by abnormally high blood sugar levels. Short-term side effects include increased thirst, frequent urination, and weight changes. Long-term complications include numbness of the hands and feet, loss of vision, kidney failure, as well as hardening of the arteries leading to amputation, heart attack, stroke, and premature death. Diabetes affects about one million Floridians and 16 million Americans. It is the leading cause of blindness in America among adults. Several studies have proven that strict control of blood sugar levels dramatically decreases the risk of blindness and other complications of diabetes. The National Eye Institute proved that laser treatment may save vision if diabetic eye damage is detected early. The American Diabetes Association recommends annual eye examinations for all adults with diabetes to prevent blindness.
Stages of diabetic retinopathy:
Non-proliferative diabetic retinopathy: The first stage of retinal damage consisting of a weakening or blockage of tiny blood vessels, which does not require treatment with laser unless macular edema develops.
Diabetic macular edema: Swelling of the central retina (the macula) due to abnormal leakage of fluid from small blood vessels weakened by diabetes. Blurring of central vision may advance to legal blindness.

Proliferative diabetic retinopathy: The second stage of diabetic retinopathy in which abnormal, weak blood vessels begin to grow from the retina into the clear gel (vitreous) which fills the inside of the eye. If not treated, this serious stage often results in loss of vision from vitreous hemorrhage. Symptoms include new “floaters” or sudden loss of vision. Retinal detachment may occur from diabetic scar tissue, which pulls the retina off the eye wall. Retinal detachment causes a dark shadow in the vision or total loss of vision. Laser and vitrectomy surgery best control these problems if detected early.


How is diabetic retinopathy diagnosed?
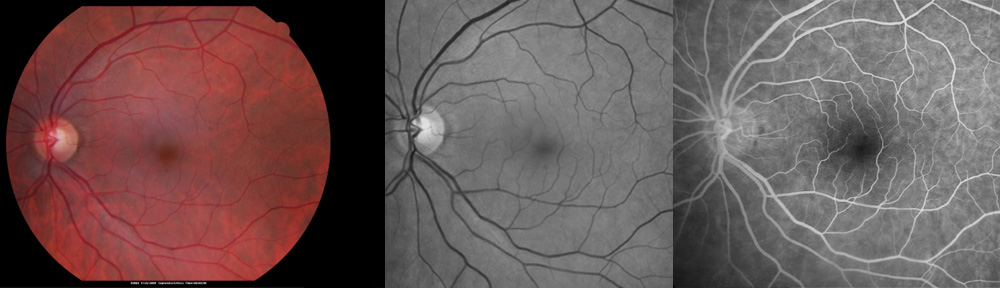
Because no symptoms may be present until severe damage to the retina has occurred, it is essential that all adults with diabetes have a complete, dilated eye examination at least once a year. The eye doctor can see into the eye with an ophthalmoscope to diagnose retinopathy. If significant changes are found, photographs can be taken to record the changes. A fluorescein angiogram may be performed in the office by injecting a fluorescent dye into the vein of the arm while photographs are taken of the retina. It supplies important information about the health of the retinal blood vessels.
How is diabetic retinopathy treated?
No treatment is needed if the vision is not threatened. If blood vessel damage is significant, painless injections of medicine (Avastin, Lucentis, Eylea, Vabysmo, triamcinolone, Ozurdex, or Iluvien) may be required to improve vision. Laser treatment performed in the office can often prevent severe visual loss. Laser produces heat, which serves to cauterize the damaged retinal blood vessels. Usually there is no pain, but if extensive laser is needed, an anesthetic injection may be given around the eye. The retinal specialist will recommend injection or laser depending on a number of factors in a given case. In severe cases of bleeding and scar tissue formation, vitrectomy surgery is performed as a one-day surgery in the hospital. With medication, laser, and vitrectomy surgery, most people can retain useful vision. However, some people lose vision despite all efforts with treatment. A change in medication taken by mouth may help some patients. A number of factors are considered in choosing the best treatment for any one patient.
What can I do to prevent diabetic damage?
Strict control of the blood sugar has been proven to reduce the rate of progression of diabetic retinopathy by about 70%. In addition, loss of vision can be minimized by optimal control of other health problems such as physical inactivity, obesity, hypertension (<130/<80), cholesterol (<200) and triglycerides (<150), heart failure, and kidney failure. Tobacco use is strongly discouraged. Daily aspirin use is recommended.
PREVENT BLINDNESS THROUGH GOOD MANAGEMENT OF DIABETES AND REGULAR DILATED EYE EXAMINATIONS.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida.
Copyright © 2022-2023 Designs Unlimited of Florida. All Rights Reserved.