See Anatomy of the Eye
What is PVR?
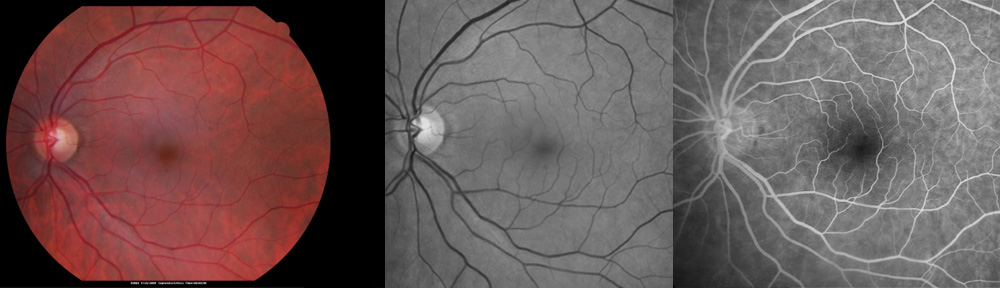
The retina is a “tissue-paper” thin layer of nerve tissue that lines the inside of the eye like the film in a camera. In the eye, light is focused onto the retina, which “takes the picture” and sends the image to the brain. Proliferative vitreoretinopathy is a condition in which sheets of scar tissue grow on the surface of the retina. It usually occurs after retinal detachment as a part of the healing process. Unfortunately, the PVR scar tissue pulls on the retinal and is the most common cause of failure of attempted repair of retinal detachment. There is evidence of PVR in about 10% of eyes that present with retinal detachment.
What is retinal detachment?
When the retina detaches, it is no longer in proper position inside the eye. Instead, it is like film that has unrolled inside a camera. When this occurs, a camera cannot take a picture. Similarly, when the retina detaches the eye loses vision.
What causes PVR?
Proliferative vitreoretinopathy is caused by the excessive formation of scar tissue. Scar tissue is a common healing mechanism in the body. For example, if the skin is cut, scar tissue closes the laceration. In the eye scar tissue develops in response to retinal detachment and surgical repair. If it becomes excessive, the scar tissue causes the retina to detach again. The abnormal production of scar tissue in the eye is called PVR. Tobacco use may increase the risk of PVR.
How is PVR treated?
The treatment of PVR requires one or more surgeries. Your doctor is skilled in a number of techniques to prevent blindness. Which type of surgery is recommended depends on the precise findings on examination.
Scleral buckle surgery: Some retinal detachments require the placement of a permanent plastic supporting belt around the eye to create a “ledge of support” for the retina. This belt is placed in the hospital operating room in a major surgery. The eye is often rendered more near sighted by this procedure. Rarely, side effects include double vision.
Vitrectomy surgery: Performed in the hospital operating room as a major eye surgery, vitrectomy surgery involves making small incisions into the eye to remove floaters, dissect scar tissue, remove fluid from under the retina, apply laser, and place a gas bubble or silicone oil into the eye to hold the retina in place. Specific head positioning is sometimes needed. Sometimes a cataract or lens implant must be removed to adequately repair the retina. After surgery, it may be necessary to lie in a specified position for several days for success. This surgery may be repeated if necessary to prevent blindness.
With one or more surgeries most retinal detachments with PVR can be repaired keeping useful vision. The vision usually does not return to normal. It is frequently blurred or distorted. There are always risks to surgery including hemorrhage, infection, scarring, glaucoma, cataract, and double vision. Sometimes despite all efforts with surgery, all vision may be lost. Surgery is recommended for retinal detachments with PVR because blindness usually results if treatment is withheld. If you have questions, please do not hesitate to ask your doctor.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida.
Copyright © 2017-2023 Designs Unlimited of Florida. All Rights Reserved.