What is Byooviz?
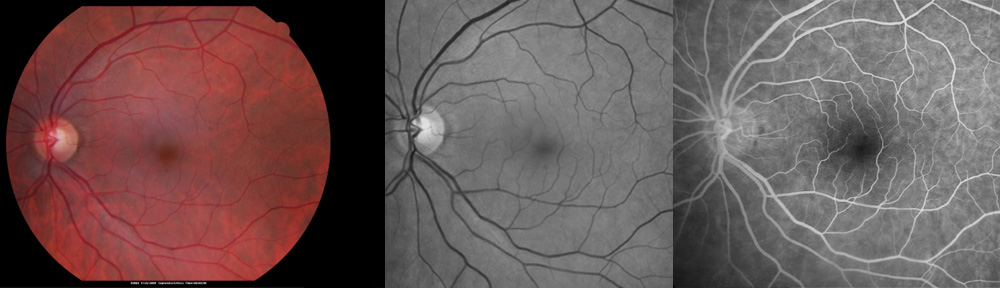
Byooviz is a drug used to treat wet-type macular degeneration, wet-type myopic macular degeneration, and macular edema due to retinal vein occlusion. It involves repeated injections of medication into the eye to stop abnormal, leaky blood vessels. Byooviz is an FDA-approved biosimilar drug similar to Lucentis. Consequently, it costs less than Lucentis (About $1100 per injection of Byooviz compared with $1800 per injection with Lucentis). Unlike Lucentis, Byooviz is not approved for diabetic retinopathy.
What is the difference between biosimilar drugs and generic drugs?
While generic drugs are chemically identical with trade-name drugs, biosimilars are not identical to their reference drugs which they attempt to duplicate. Because biosimilar drugs are different chemically, they may behave differently in terms of effectiveness and side effects. They may not be as effective as their reference drug and they may have more side effects. For this reason, biosimilar drugs need to be monitored closely prior to approval by the FDA, as well as after approval by health care providers. Some adverse effects are not recognized until a drug has been used in thousands (if not more) of patients.
How effective is Byooviz therapy?
Byooviz was shown to be very effective and similar to Lucentis when given every 4wks up to 48 weeks for wet-type macular degeneration. Currently, therapy often starts with monthly injections until maximal vision is restored. Afterwards, the injections may be given less frequently to maintain stable vision. It is not known how Byooviz will perform in this setting.
What are the risks of Byooviz therapy?
Severe complications are very rare, but risks of Byooviz injection (like Lucentis) include bleeding, infection, retinal detachment, glaucoma, cataract, and loss of vision/loss of the eye. There appears to be a small increased risk (1%) of stroke with these types of medications. The risk of stroke may be related to the older age of patients in which it is used. Pregnancy should be avoided while on Byooviz therapy.
What do I expect after a Byooviz injection?
Be careful not to rub the eye after the injection because the eye may remain anesthetized for several hours. You may be given eye drops and instructions on how to use them. Physical activity is not limited after the injection. Tylenol or Ibuprofen may be used if there is discomfort, but severe pain should be reported to your doctor without delay. It is normal to experience a red area on the white of the eye, which disappears in one to two weeks. If you have any questions or concerns, please call the office.
What does Dr Pautler think about Byooviz?
It is the opinion of the author that there are several concerns about Byooviz. First, the safety and effectiveness of Byooviz need to be determined on a large scale with many more patients than studied for FDA approval. This may take several years of use. Until then, I prefer Lucentis as it has a proven track record. Secondly, the cost of Byooviz appears too high. The cost of Byooviz is less than Lucentis, but not by much. A lower cost is more appropriate given the unknown risks and long-term effectiveness of Byooviz. If I have a patient whose insurance covers Lucentis, that is my choice over Byooviz at this time. If a patient has a Medicare Advantage insurance plan, I may be forced to use Byooviz.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida with the exception of limited one-time consultations with residents of the following states: Alabama, Arkansas, Connecticut, Georgia, Minnesota, and Washington.
Copyright ©2022 Designs Unlimited of Florida. All Rights Reserved