What is endophthalmitis?
Endophthalmitis (“end-off-thal-my-tis”) is a severe inflammation inside the eye. The inflammation may be due to an infection or it may be “sterile.” Endophthalmitis threatens profound loss of vision and possible loss of the eye. Bacterial endophthalmitis usually requires urgent treatment to save the eye.
What causes endophthalmitis?
Endophthalmitis may be caused by an auto-immune reaction (the body attacks itself), it may be due to a foreign substance introduced into the eye in an accident or surgery, or it may be due to an infection. Here we will discuss endophthalmitis due to infection.
Infections may be caused by a number of viruses, fungi, parasites, and bacteria. Infectious endophthalmitis is classified as endogenous and exogenous. Endogenous endophthalmitis occurs when an infection enters the eye from inside the body, usually through the blood stream. Exogenous endophthalmitis occurs when an infection enters the eye from outside the body, usually from an opening into the eye from trauma, surgery, or intraocular injections.
How is infectious endophthalmitis diagnosed?
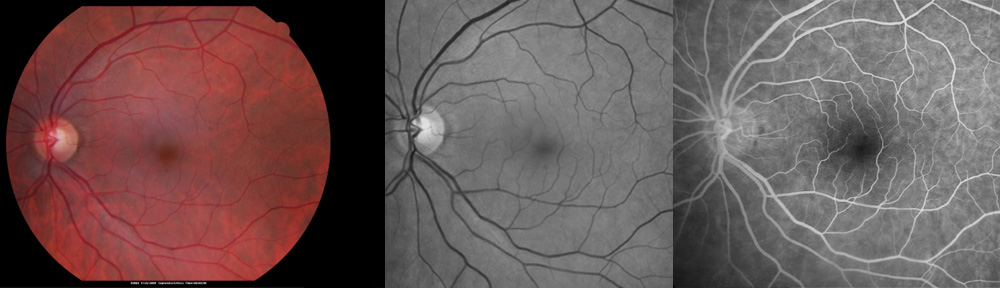
Infectious endophthalmitis is suspected when severe inflammation is found inside the eye on an exam. It is usually accompanied by pain and loss of vision. Diagnosis is confirmed with a culture of the fluid inside the eye taken in the office or the operating room.
How is infectious endophthalmitis treated?
Infectious endophthalmitis is treated with antibiotic injections into the eye performed in the office or in the operating room. In severe cases, vitrectomy surgery is needed to remove some of the infected material. Vitrectomy is performed in the hospital operating room as a major eye surgery involving small incisions into the eye. Eye drops (steroid and non-steroid) are used frequently to help treat infection and to decrease the inflammation that can damage the eye. Sometimes additional steroid medications are used. The recovery of vision is very slow, taking weeks to months. If permanent damage occurs as a result of endophthalmitis, little or no recovery of vision may be possible. Frequent visits to the doctor are necessary at first to give the best results.
If you have questions, please do not hesitate to ask your doctor. Please visit www.retinavitreous.com
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida with the exception of limited one-time consultations with residents of the following states: Alabama, Arkansas, Connecticut, Georgia, Minnesota, and Washington.
Copyright © 2018-2023 Designs Unlimited of Florida. All Rights Reserved.