What side effects can pentosan polysulfate have on my eyes?
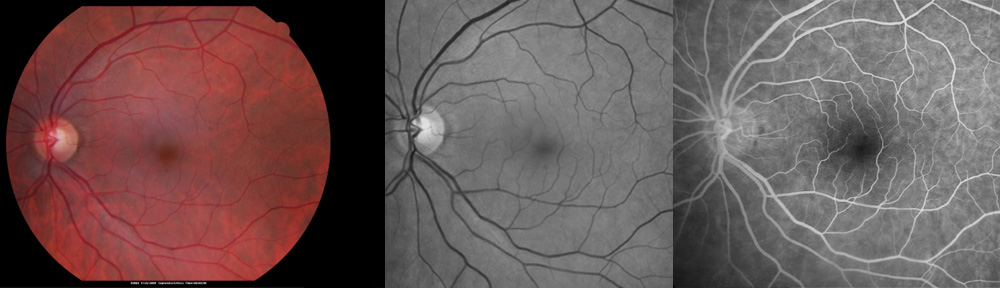
Although pentosan polysulfate (PPS) is of proven benefit for interstitial cystitis, it may cause damage to the eyes. Early symptoms may be subtle. Blurred vision, especially with reading, is common. Straight lines may appear wavy or distorted. There may be a slow adaptation from light to dark environments. Blind spots or missing areas may occur in the central vision. These symptoms are due to retinal damage; however, they are not specific to pentosan polysulfate damage. The Eye MD (retina specialist) must use special tests to determine whether vision symptoms are due to pentosan polysulfate or other types of retinal conditions such as macular degeneration.
Who is at risk of losing vision?
Ocular side effects appear to be related to a build-up of medicine in the body over years. The longer a person has been on PPS, the greater the chances of developing retinal damage. Although the average duration of use at the time of diagnosis is 15 years, some patients develop symptoms as early as three years after starting the medication. With continued use of PPS, additional permanent damage occurs that may result in loss of vision.
What can I do to protect myself?
Pentosan polysulfate is an effective medication for control of pain with interstitial cystitis. However, it is important to monitor your eyes for side effects that might indicate the need to stop the medication. The Amsler grid chart should be checked at least once a week testing each eye separately, using glasses if needed. Look for a missing part of the grid either above or below the central dot while looking only at the center of the grid. Additionally, your Eye MD should examine your eyes every year with specific testing to look for early signs of retinal changes. It may be useful to see a retinal specialist who has training in this area.
What happens if I develop retinal changes from pentosan polysulfate?
If early retinal changes are found, pentosan polysulfate may be discontinued. By discontinuing pentosan polysulfate at an early stage, vision may be saved. Continued examination is important to monitor the eyes for further changes. There is no specific treatment for retinal toxicity from pentosan polysulfate. However, if blood vessels grow under the retina, treatment may be helpful as with wet macular degeneration.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida with the exception of limited one-time consultations with residents of the following states: Alabama, Arkansas, Connecticut, Georgia, Minnesota, and Washington.
Copyright © 2019-2022 Designs Unlimited of Florida. All Rights Reserved.