What is visual snow?
Visual snow is the name for a visual symptom that looks like static on a television not tuned to a station. It has also been likened to pixelation on a computer screen. Many tiny flickering lights are usually seen in both eyes at the same time and encompasses the entire visual field. In some instances, it is worse in bright illumination like a bright sunny day.
What is the difference between primary and secondary visual snow syndrome?
Visual snow may be seen in patients without an underlying disease. In these cases it appears to be caused by hyperexcitability of the visual cortex of the brain. This is often called primary visual snow syndrome (VSS). Primary VSS is a diagnosis of exclusion. That is, other diagnoses must be excluded before the diagnosis of primary VSS is made. Primary VSS is related to migraine; indeed, many people who report visual snow also have migraine visual symptoms with or without headache. Other related symptoms include palinopsia (visual persistence of an image after the eyes are closed or look away), floaters and spots (entopsia), difficulty seeing in dim light (nyctalopia), difficulty seeing in bright light (hemeralopia), and flashes of light (photopsia). Other associated symptoms include ringing in the ears (tinnitus) and dizziness that varies with head position (postural vertigo).
Visual snow may be a symptom of an underlying disease (secondary visual snow syndrome). In this situation, it is critical to identify the underlying cause and offer treatment where possible. Secondary visual snow may originate from the retina or the brain. A well-described retinal cause of visual snow is due to digoxin toxicity. It usually occurs in elderly people who take digoxin for heart problems. It indicates the need to stop taking digoxin or lower the dose. Failure to reduce the dose may result in severe complications, including death. Other rare causes of visual snow include eye disease, immune disease, infectious disease, psychiatric disease, prescription drugs, past use of hallucinogens, head trauma, brain tumor, seizure disorder, and brain degenerative disease.
What causes the primary visual snow syndrome?
The cause of primary VSS is not known. It is felt to be due to an error in central processing in the back of the brain (occipital lobe). Special brain scans show hypermetabolism in the lingual gyrus of the occipital lobe in the back of the brain.
How is primary visual snow syndrome diagnosed?
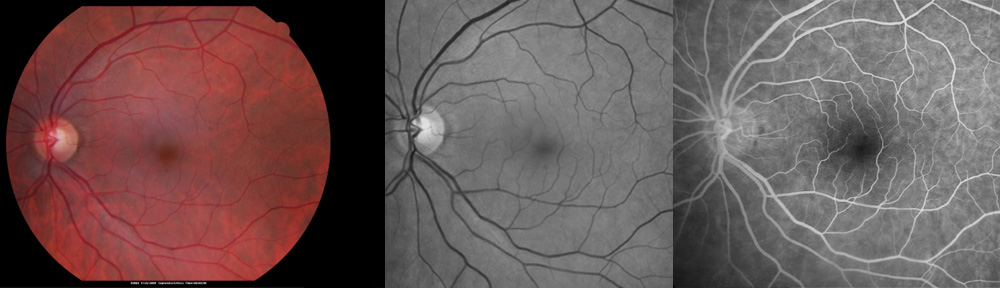
The diagnosis is made on the basis of typical symptoms after testing has ruled out an underlying disease of the eye or brain. MRI brain scan is often used to rule out tumor, multiple sclerosis, degeneration, and stroke. EEG may be used to rule out seizure disorder. A spinal tap may be needed to rule out idiopathic intracranial hypertension. Pattern reversal VEP usually demonstrates loss of habituation of the occipital lobe in the brain (indicative of hyperexcitability). A neurologist usually arranges for testing as needed. An ophthalmologist may be helpful in ruling out eye disease.
What can be done about these symptoms?
It is difficult to treat primary VSS. Medications such as lamotrigine and topirimate may be helpful in some patients. Tinted glasses or clip-on lenses may also be helpful to minimize the symptoms of visual snow. Placing a yellow or orange tinted cellophane sheet on top of reading material helps some. Riboflavin and magnesium supplements may be of benefit for migraine and visual snow, as well. For many patients it is helpful to know that primary VSS is a benign condition that does not progress to blindness.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida.
Note: This blog is supported by its readers via small commissions that may be earned through hyperlinks. The commissions do not increase the price you pay and do not affect the content of this article. Thank you for your support.
Copyright 2022-2023 Designs Unlimited of Florida. All Rights Reserved.