What is hypermetropia?
A hypermetropic eye is a far-sighted eye. Without glasses the vision may be good at distance or blurred, but the vision is usually blurred or strained at near without glasses. Hypermetropia is different from presbyopia (aging eyes). Hypermetropia affects many people and is treated with glasses, contact lenses, and, rarely, laser surgery. It is a common underlying reason for the need to wear optical correction (glasses).
What causes hypermetropia?
Hypermetropia is an inherited condition that usually develops in childhood or early adulthood. The eye develops with either a flat cornea or a short eyeball length, or both. As a result, the image entering the eye is focused behind the plane of the retina. In this case, the eye tries to focus the lens to make the image projection sharp. Sometimes, the natural lens in the eye can compensate for the focusing of images, but often eyeglasses or contact lenses are needed. The outer appearance of the eye is not usually changed. It is not obvious that an eye is hypermetropic by inspecting the outside of the eye.
Why is it important to know about hypermetropia?
Although most people with hypermetropia do not develop complications, some far-sighted people are at increased risk of losing vision from narrow-angle glaucoma, central serous choroidopathy (also known as central serous retinopathy), and choroidal effusion.
Angle-Closure Glaucoma is a condition in which the pressure inside the eye damages nerve tissue that helps you see. High pressure is the result of closure of the internal drain in the eye. The pump inside the eye does not sense the closure of the drain; it continues to pump fluid into the eye. The drain cannot keep up with the pump, so the pressure inside the eye rises. This pressure may or may not cause pain or discomfort. Over time, the pressure slowly takes away the side vision. If undetected and untreated, it may cause total, irreversible blindness. The best way to diagnose glaucoma is to have regular eye exams each year with pressure measurements and gonioscopy. Treatment is effective in preventing vision loss. Laser is often used to open the drain. Sometimes operative surgery is required with or without removal of the lens in the eye (to make more room for the drain to stay open). Often, eye drops are needed long-term to keep the pressure under control.
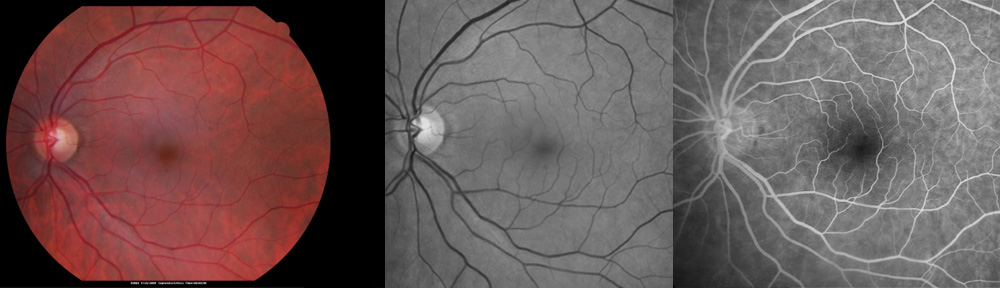
Central Serous Chorioretinopathy is an uncommon cause of vision loss from hyperopia. The retina is a thin layer of delicate nerve tissue that lines the inside wall of the eye like the film in a camera. In the eye, light is focused onto the retina, which “takes the picture” and sends the image to the brain. In hypermetropic eyes, the layer under the retina called the choroid becomes crowded and thickened. The outer coat of the eye known as the sclera may be thickened as well. As a result of thickened choroid and sclera, the flow of fluid inside the eye that normally drains out through these structures, is restricted. This fluid may then collect under the retina and cause the central vision to become blurred or distorted even with proper glasses. Distortion is when straight lines look wavy or crooked. Blood vessels under the macula may bleed causing sudden blurring, blind spot, or distortion. Any of these symptoms should be reported to the eye doctor without delay, as early treatment with laser may prevent further loss of vision.
Choroidal Effusion is a separation of the choroid from the sclera, the wall of the eye. This is different from retinal detachment. When the choroid detaches, it is no longer in proper position inside the eye. As a result, symptoms of a dark curtain or shadow slowly starts off to the side and takes away the vision as the choroid detaches. Pain is not common. The diagnosis is made by a retinal specialist; it is critical to identify and differentiate choroidal detachment from retinal detachment and tumors. Treatment of choroidal effusion is typically started with medications. Sometimes, however, surgery is needed.
Will refractive surgery help prevent these complications of hypermetropia?
Although refractive surgery (laser correction) is effective at changing the shape of the cornea to help eliminate the need for corrective lenses (glasses and contacts lenses), it does not restore the natural shape of the eye. Therefore, it is still necessary to be aware of the warning signs of possible complications from hypermetropia.
What should a hypermetropic patient do?
Using your eyes to read or work at a computer will not weaken them. Remember to have your eyes examined once a year with special attention to the opening of the drainage apparatus (the corneoscleral angle). Not all eye doctors are proficient with determining the risk of angle-closure glaucoma; therefore, consider seeing a fellowship-trained glaucoma specialist if needed. In Tampa there are several choices including doctors Levitt, Gamell, Richards, King, and Fridman. Apart from an annual exam, report the following symptoms to your eye doctor without delay:
Sudden-onset pain in the eye (sometimes, associated with nausea)
Sudden-onset redness (especially, if associated with pain and blurred vision)
Loss of side-vision (possibly, a very late sign of glaucoma)
| Copyright © 2022 Designs Unlimited of Florida. All Rights Reserved. |
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida with the exception of limited one-time consultations with residents of the following states: Alabama, Arkansas, Connecticut, Georgia, Minnesota, and Washington.