What is inflammatory bowel disease?
Inflammatory bowel disease includes conditions such as ulcerative colitis and Crohn’s disease. They are inflammatory conditions not caused by infection. Instead, the immune system appears to mistakenly attack the bowel. The same immune cells may also attack the eye in these bowel conditions. Ocular inflammation is called uveitis. And the most common type of uveitis caused by inflammatory bowel disease, is intermediate uveitis.
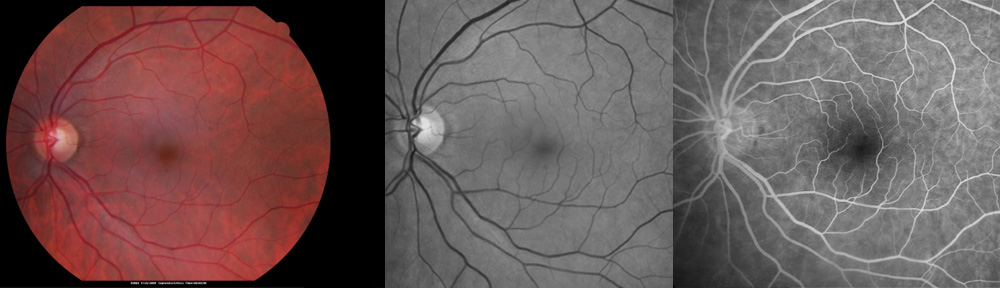
Uveitis (pronounced, “you-vee-EYE-tis”) is a general term used to describe inflammation inside the eye. The uvea is the name given to the layer of tissue in the eye that has a brown color (melanin pigment) and blood vessels, which serve to provide blood supply and protect the eye from excessive light (see anatomy of the eye). The uvea can be divided into separate parts, which perform different functions in the eye: the iris, the ciliary body, the pars plana, and the choroid. The part of the uvea in the front of the eye is called the iris (the round, blue or brown part of the eye that you can see in the mirror). Behind the iris is the ciliary body, which produces the fluid that fills the eye. The pars plana serves as the boundary between the ciliary body and the choroid. The back part of the uvea that lies under the retina (the “film” in the eye that “takes the picture”) is called the choroid. Therefore, in any one patient uveitis is usually given a more specific name depending on where most of the inflammation is located in the eye. In intermediate uveitis the inflammation is primarily located in the vitreous gel that fills the eye, which is located in an intermediate position between the front and the back of the eye. It is sometimes referred to as vitritis.
What are other causes of intermediate uveitis?
Uveitis may be caused by an infection, an injury from trauma, a disease in the body outside the eye, or sometimes for unknown reasons. Infection by a virus, bacteria, fungus, or other parasite may cause uveitis. Infections may be limited to the eye or may involve other organs as well. In intermediate uveitis, infection may be caused by syphilis, tuberculosis, Lyme disease, cat scratch disease, Whipple’s disease, toxocariasis, human lymphotrophic virus (HTLV-1), or toxoplasmosis.
In other situations, uveitis is caused by inflammation without infection. For example, multiple sclerosis and sarcoidosis may cause intermediate uveitis. Pars planitis is a sub-type of intermediate uveitis that often starts early in life during childhood. Its cause is unknown.
Uveitis commonly occurs following an injury to the eye. Very rarely, cancer or cancer-fighting drugs may cause intermediate uveitis. In some cases, no underlying cause can be found to be the cause of uveitis. Tobacco may be an aggravating factor and should be discontinued.
What are the symptoms of intermediate uveitis?
The most common symptoms include tiny floating spots which move or “float” in the vision. They are usually numerous and may cause a veil-like appearance in the vision. Sometimes blind spots, blurred vision, distortion, or loss of side vision occurs. The eye may be painful, red, tearing, and light sensitive if other parts of the eye are also inflamed. Symptoms may be mild or they may be severe and disabling.
How is intermediate uveitis managed?
Treatment of the underlying inflammatory bowel disease will also help treat the uveitis. Separately, it is important to find any other underlying cause whenever possible. Take some time to carefully review and report to your doctor any unusual or unexplained symptoms such as rashes, back and joint problems. Tell your doctor if you travel abroad, spend time in rural settings, or may be exposed to animals or infections. Heredity may also play a role. You should tell your doctor about any family members with inflammatory disorders anywhere in the body. Also, review and report your ancestry (for example, Asian, Mediterranean, or American Indian ancestry). When the doctor diagnoses uveitis, laboratory tests may be ordered to help determine its cause. Occasionally, a surgical biopsy is needed for diagnosis. If infection is found, antibiotics are prescribed. To limit the damage from inflammation, intermediate uveitis is treated with anti-inflammatory medication in the form of eye drops, injections, or pills. When pills are used, the eye doctor frequently coordinates medical care with the expert assistance of a rheumatologist. Rarely, surgery is required to treat uveitis. In some cases, intermediate uveitis may be long-lasting. In these cases, years of therapy are needed to preserve vision. Intermediate uveitis is a serious eye problem and may result in loss of vision or blindness. However, by seeing your eye doctor and taking the medications exactly as recommended, damage to your vision can be minimized.
In some cases, intermediate uveitis may go away, but return at a future date. Therefore, if you become aware of symptoms of uveitis in the future, do not hesitate to contact your doctor. Preliminary evidence suggests that tobacco use may be an aggravating factor in some cases of uveitis. Also, vitamin D supplements may be helpful.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida with the exception of limited one-time consultations with residents of the following states: Alabama, Arkansas, Connecticut, Georgia, Minnesota, and Washington.
Note: As an Amazon Associate I may earn from qualifying purchases. You pay no additional fees by accessing the link. These funds help defray the costs of maintaining this website. Thank you for your support of the blog.
Copyright © 2021-2022 Designs Unlimited of Florida. All Rights Reserved.