What is polypoidal choroidal vasculopathy (PCV)?
Polypoidal choroidal vasculopathy (PCV) is a type of age-related macular degeneration (AMD), the most common cause of visual loss in older Americans. The macula is the area of the retina in the back of the eye that is responsible for seeing details in the central vision. The retina is a thin layer of delicate nerve tissue that lines the inside wall of the eye like the film in a camera. In the eye, light is focused through the lens onto the retina, which “takes the picture” and sends the image to the brain. PCV is a disease that affects the central vision. It does not affect peripheral vision— the ability to see objects off to the side when looking straight ahead. This means that PCV alone does not result in total blindness.
In PCV, abnormal blood vessels grow under the macula from a deep layer of normal blood vessels (the choroid). The normal blood vessels in the choroid are usually separated by a tissue membrane from the macula. However, in PCV abnormal blood vessels start growing from the choroid and invade the tissue beneath the macula. These abnormal vessels leak fluid and blood under the macula causing loss of vision.

What causes polypoidal choroidal vasculopathy (PCV)?
Polypoidal choroidal vasculopathy appears to be an inherited condition. PCV may occur in anyone, but it is more common in people who descended from Asia or Africa. Therefore, genetic factors likely play a role in the cause of PCV. It may be aggravated by factors that cause hardening of the arteries like aging, high blood pressure, high cholesterol, overweight, physical inactivity, and tobacco use.
Before abnormal blood vessels grow under the macula, there are usually findings that predict eyes that are at risk of developing PCV. For example, the choroid (normal blood vessel layer under the macula) is usually thicker than average. A thicker choroid may result in higher blood flow beneath the macula that may cause the growth of abnormal blood vessels. In addition, pale deposits (drusen) may appear under the macula prior to the development of abnormal blood vessel growth. These deposits may contain waste products of cellular function, as well as cholesterol. Perhaps, newly growing blood vessels are called on by the macula to clear away the waste deposits. Regardless, the abnormal blood vessels threaten loss of vision due to leaking, bleeding, and scarring beneath the macula.
What are the symptoms of polypoidal choroidal vasculopathy (PCV)?
Polypoidal choroidal vasculopathy may cause no symptoms in its early stages, especially if the abnormal blood vessels are located away from the center of the macula or if they have not begun to leak significantly. Eventually, symptoms may include distortion of central vision or a blind spot in the vision.
How is polypoidal choroidal vasculopathy (PCV) diagnosed?
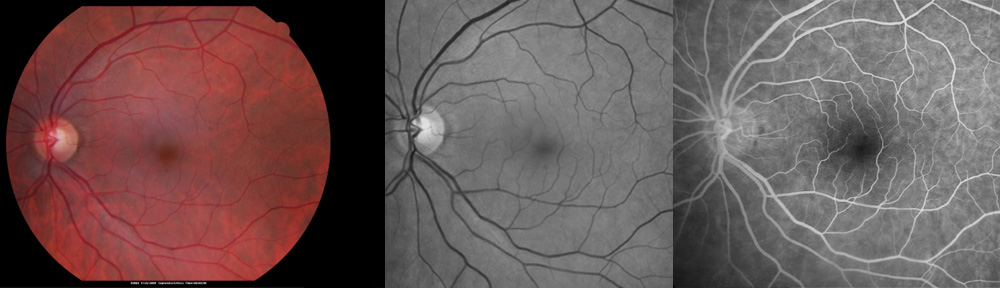
A dilated eye examination can often detect changes in the macula before visual loss occurs from PCV. The hallmark of PCV, as well as other forms of macular degeneration, is the presence of drusen—tiny yellow deposits of waste products from the retinal cells that appear as spots under the retina. After the diagnosis is made, a fluorescein angiogram may be needed. This is a procedure where the ophthalmologist injects an organic dye into the vein of a patient’s arm. Then, photographs of the retina show the presence and location of the leaking blood vessels marked by the organic dye.
How is polypoidal choroidal vasculopathy (PCV) treated?
There is evidence that taking vitamin/mineral supplements in specific dosages decreases the risk of visual loss from PCV. For high risk eyes, the following supplement is recommended: Preservision Soft Gels AREDS 2 Formula one capsule twice-a-day. To avoid toxic side effects, be careful about taking additional vitamins or zinc. However, you may take calcium, iron, and vitamin D if recommended by your doctor for problems not related to your eyes. Check pricing of Preservation on Amazon.
People with PCV can often be helped with medication injections and a special laser (PDT) performed in the office. The Everest Study found that the combination therapy with medication injection and PDT (photodynamic therapy) was more effective than medication injection alone. The combination treatment group recovered more vision and required fewer treatments by injection. This treatment regimen differs from other types of age-related macular degeneration.
Treatment rarely returns vision to normal, but may limit the amount of vision loss from blood vessel growth and leakage. Frequent office visits and photographs are needed. It may be useful to stop smoking, avoid becoming overweight, exercise daily, and control blood pressure and cholesterol. Aspirin should only be used if required to treat disease as recommended by a doctor. Relatives should be checked for polypoidal choroidal vasculopathy, as well.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida with the exception of limited one-time consultations with residents of the following states: Alabama, Arkansas, Connecticut, Georgia, Minnesota, and Washington.
NOTE: As an Amazon Associate I may earn from qualifying purchases. You pay no additional fees by accessing the link. These funds help defray the costs of maintaining this website. Thank you for supporting this blog.
Copyright © 2021 Designs Unlimited of Florida. All Rights Reserved.